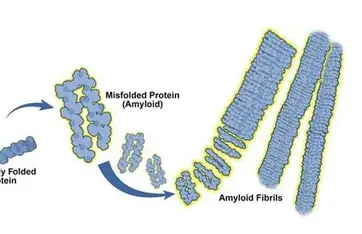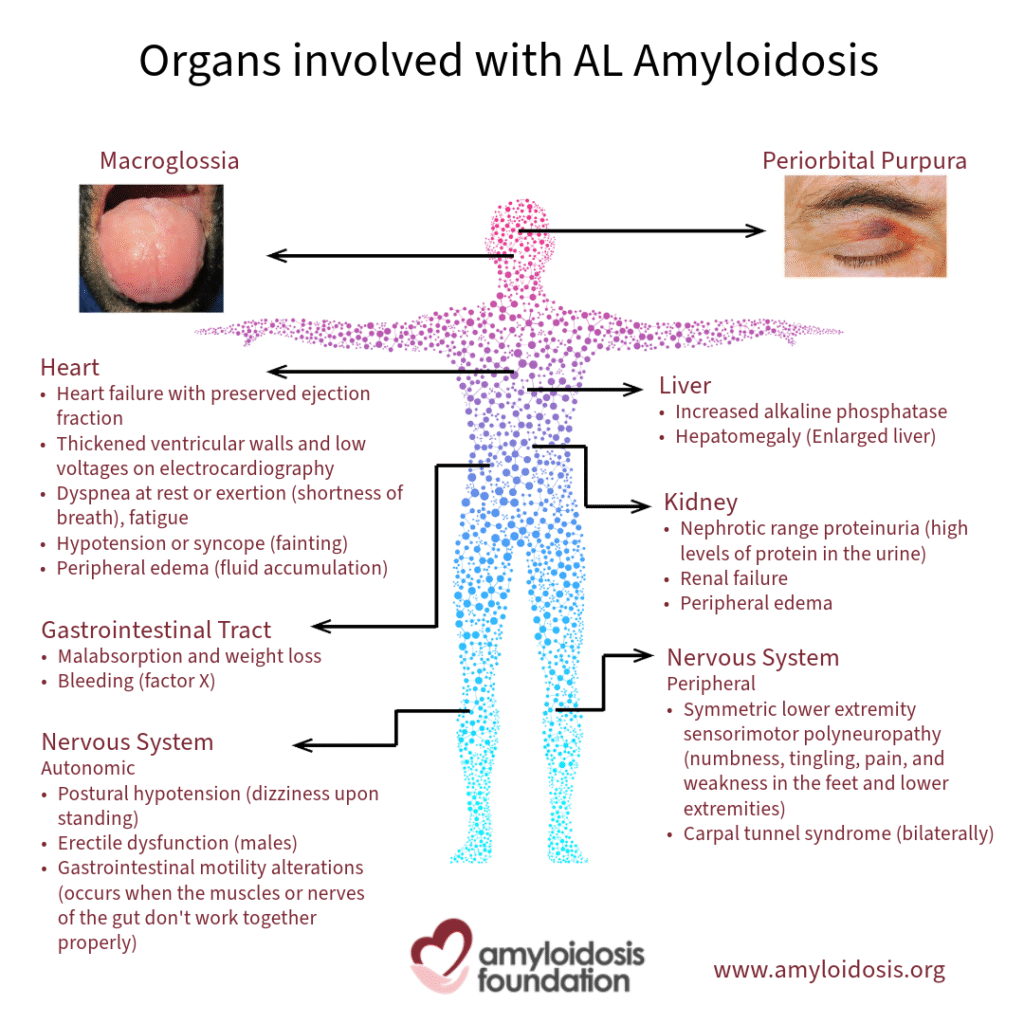
AL amyloidosis, also known as light-chain amyloidosis, is a rare but serious disorder caused by abnormal plasma cells in the bone marrow. These cells produce misfolded immunoglobulin light chains that accumulate as amyloid deposits in vital organs such as the heart, kidneys, liver, and nerves. Over time, these deposits interfere with normal organ function and can become life-threatening if not diagnosed and treated early.
What Makes AL Amyloidosis So Challenging?
One of the biggest challenges with AL amyloidosis is delayed diagnosis. Early symptoms are often vague and overlap with common conditions—fatigue, swelling in legs, breathlessness, foamy urine, numbness, or unexplained weight loss. Many patients are diagnosed only after significant organ damage has already occurred, especially to the heart or kidneys.
Recent research highlights that earlier detection is critical, as outcomes are strongly linked to how quickly treatment begins.
Recent Research Insights (2023–2025)
New scientific studies have significantly improved understanding of AL amyloidosis at the cellular level. Researchers have found that the bone marrow environment in AL amyloidosis is highly inflammatory, which contributes to disease progression. Unlike multiple myeloma, AL amyloidosis plasma cells show unique stress-related genetic behavior due to the continuous production of misfolded light chains.
Another important breakthrough is the identification of high-risk patients earlier through blood biomarkers. Certain proteins and cardiac markers can indicate amyloid buildup years before severe symptoms appear. This opens the door to screening people with related plasma cell disorders and starting treatment much sooner.
Advances in Diagnosis
Diagnosis of AL amyloidosis still relies on tissue biopsy, where amyloid deposits are confirmed using specialized staining techniques. However, modern diagnostic protocols now combine:
- Sensitive blood and urine tests to detect abnormal light chains
- Advanced cardiac biomarkers for early heart involvement
- Imaging techniques such as cardiac MRI
- Precise amyloid typing using mass spectrometry
Artificial intelligence is also emerging as a powerful tool. AI-based analysis of cardiac imaging is helping doctors distinguish amyloidosis from other heart diseases faster and more accurately, reducing diagnostic delays.
Current and Emerging Treatments
Treatment for AL amyloidosis focuses on eliminating the abnormal plasma cells producing the toxic light chains.
Standard Therapy
The current first-line treatment includes combination chemotherapy with monoclonal antibodies. These regimens have dramatically improved response rates and survival, even in patients with cardiac involvement.
Targeted and Precision Treatments
For patients with specific genetic features, targeted drugs have shown excellent results, producing deep and rapid disease control. These therapies are especially effective in relapsed or treatment-resistant cases.
Immunotherapy and CAR-T Research
One of the most promising recent developments is immune-based therapy. Early clinical trials using CAR-T cell therapy have shown rapid clearance of abnormal light chains, deep remission at the bone marrow level, and meaningful improvement in organ function. These results suggest a potential future where AL amyloidosis could be controlled with a single, highly targeted treatment.
Amyloid-Clearing Therapies
Researchers are also working on treatments that directly remove amyloid deposits from organs. While some trials have shown mixed results, ongoing studies continue to explore whether clearing amyloid can reverse organ damage and improve long-term survival.
Importance of Early Detection and Multidisciplinary Care
Experts now strongly recommend that unexplained heart failure, kidney disease, or neuropathy should always be evaluated for amyloidosis. Early referral to specialized centers and coordinated care between hematologists, cardiologists, and nephrologists significantly improves outcomes.
Conclusion
AL amyloidosis research has entered a transformative phase. Advances in early diagnosis, biomarker screening, targeted therapies, and immunotherapy are reshaping the future for patients. While challenges remain, especially in awareness and access to care, the progress made in recent years offers real hope.
Early recognition, timely treatment, and continued research are the keys to improving survival and quality of life for people living with AL amyloidosis.